laboratory instruments distributor
Autoclave
Autoclave - Types of autoclave - Laboratory autoclave
What is an autoclave?
Autoclaves are also known as steam disinfectants, and are commonly used for health care or industrial applications.
An autoclave is a device that uses pressurized steam to kill harmful bacteria, viruses, fungi, and spores on devices that are placed inside a pressure vessel.
The material is heated for a certain period of time at the appropriate sterilization temperature. The moisture in the steam effectively transfers heat to the items to destroy the protein structure of bacteria and spores.
In healthcare, the term “autoclave” is commonly used as a term to describe a steam disinfectant.
ANSI / AAMI 4, which provides standards and guidelines for the processing of medical devices, refers to healthcare autoclaves specifically as steam disinfectants.
Autoclaves have 3 classes: Class N, Class S and Class B.
Class N = Commonly used for solid tools without coating. Not used for sterile coated and perforated items (such as cloth).
Class S = This model is the same as Class N for solid tools, except that it is used for both coated and uncoated devices and perforated devices. It also has a vacuum pump and a drying cycle.
Class B = In this model, in addition to providing all class N and S coatings, it also covers textile materials. Autoclaves in this class have a powerful vacuum pump that creates a vacuum of up to -0.9 times.
Who Invented the Autoclave?
The prototype autoclave, now known as the laboratory autoclave, was invented in 1679 by French-born physicist Dennis Papin. It was not until 1879 that the French microbiologist Charles Chamberlain introduced a new version called the autoclave for use in medical applications.
The science of disinfection and sterilization began in 1881 with Robert Koch’s research on steam and hot air disinfection. He showed greater penetration power shown by wet heat (steam) compared to dry heat.
Finally, in 1933, modern autoclave technology was introduced with the first pressurized steam disinfectant that controlled performance by measuring the temperature in the discharge line of a chamber (thermostatic trap). Prior to this date, pressure was the only control indicator without any means of temperature verification or air removal.
Over time, new autoclave technology, including pre-vacuum cycles in 1958 and steam washing pulse pressure, was developed in 1987, allowing science to use in autoclaves or steam disinfectants in hospitals today. Used, evolve.
Types of autoclave models
Laboratory autoclave
- Produced in volumes of 10-25-50-75 and 100 liters
- The device is made entirely of steel (door, crown, tank and cover of the device)
- Equipped with PWM digital panel
- This system has high efficiency energy consumption optimization and waste temperature control system for the element
- Equipped with electronic system to control the water level (power outage in case of water shortage)
- Autoclave with Italian safety valve with CE certification and Italian performance certification
- The unbreakable and antibacterial lid houses the clips
- Laboratory autoclave with P.W.M digital board has one year warranty and ten years after-sales service.
Hospital autoclave
- Hospital autoclave is produced in two forms: single door, double door.
- Has a digital electronic board
- It has a working cycle at 121 and 134 ° C
- Mechanical pressure
- 12 kW power consumption is three-phase
- Room air inlet with HEPA filter (biological filter)
- Italian safety valve with CE certification and Italian performance certification
- 4 mm thick sheet with 4 mm thick jacket
- Produced in dimensions of 200 and 300 liters
- This hospital disinfectant has a 12-month warranty and a ten-year after-sales service.
- It has ISO 13485 (standard for quality management of medical equipment) and ISO 9001
Clinical autoclave
- Has a fully automatic door and the ability to open the door manually
- Stainless steel body with scratch-resistant electrostatic coating
- Fully electronic smart board (device error announcement on LCD)
- The room air inlet is equipped with a HEPA filter
- Has a separate dryer
- Report capability via printer cable and USB port output
- Fast cycle This includes a sensor to detect water quality
- It has 5 work cycles:
- Prion program 134 degrees Celsius Fast program 134 degrees Celsius
- ° World program 134 ° C Quiet program 121 ° C
- Laboratory 121 ° C
- By vapor permeability test (B&D) and vapor leakage test (vacuum test)
- It has a fast steam generator
- Italian CE certified safety valve and vacuum pump uum 0.8 times Korean
- It has the standard seal of ISO 13485, ISO 9001

Dental autoclave
- Has a fully automatic door and the ability to open the door manually
- Dental autoclave with all-steel tank, steel sheet body with electrostatic paint, scratch-resistant
- Has a completely Persian smart electronic board (device error announcement on LCD)
- Desktop autoclave with 5 work cycles:
- Prion 134c program Fast 134c program
- World Program 134c Quiet Program 121c
- Laboratory program 121 c
- With vapor permeability test (B&D) and vapor leakage test (uum vacuum test)
- Dental autoclave with fast steam generator
- Room air inlet equipped with HEPA filter
- Has a separate dryer
- Italian CE certified safety valve and Korean Korean vacuum pump with 0.8 bar vacuum power
- It has a standard stamp, ISO 13485, ISO 9001 and approval of the General Directorate of Medical Equipment
- Desktop, horizontal, digital, Class B (electric door) dental autoclave has one year warranty and ten years after-sales service.
How does an autoclave work?
Autoclaves are commonly used in sanitary settings to sterilize medical devices.
Items that need to be sterilized are pressurized inside a tank, commonly called a chamber.
Three factors are critical to ensuring successful steam sterilization in an autoclave: time, temperature, and steam quality.
To meet these needs, there are three steps to the autoclave process:
1) How to use steam
2) How to use air and dry heat
3) Plasma method and other methods
Quality steam is critical to a successful autoclave sterilization process. The steam used for sterilization should consist of 97% steam (steam) and 3% moisture (liquid water). This ratio is recommended for the most efficient heat transfer.
When the steam humidity is less than 3%, the steam is described as too hot (or dry). Too hot steam is too dry for effective heat transfer and ineffective for steam sterilization.
What is the autoclave temperature range?
The typical temperature for steam sterilization is 250 degrees Fahrenheit (121 degrees Celsius), 270 degrees Fahrenheit (132 degrees Celsius) or 275 degrees Fahrenheit (135 degrees Celsius).
To kill existing microorganisms, items to be sterilized must be exposed to this temperature for at least the time recommended by the manufacturer of the processing machine.
What is the time frame of the autoclave cycle?
Exposure time is the time required to sterilize the device and does not cover the entire cycle time. There is a time / temperature relationship for proper steam sterilization that has been established by scientific experimentation and is used in all sterilization methods to create what is known as the total exposure step.
Periods of steam exposure for steam sterilization are other factors depending on the size, shape, weight, density and material composition of the device being sterilized.
What is the size of the autoclave?
The size of the disinfectant will vary depending on the capacity required for the autoclave area.
For example, in an autoclave dental office it may be easy to place a desk where equipment is only needed to sterilize small tool kits.
Immediate disinfection is usually needed in the operating room, and may only require processing 1-3 tool trays at a time. However, most health centers have large autoclaves in the sterile processing unit (SPD) that can process up to 15-20 trays of tools per cycle or even up to 625 pounds of instruments per cycle.
Industrial-sized autoclaves for manufacturing processes can be very large, some comparable to the size of a semi-truck or aircraft.
Uses of autoclave
Devices must be compatible with the autoclave process. Autoclaved items must be compatible with high heat and humidity conditions and processed according to the instructions used by the manufacturer.
Medical devices that come into contact with sterile body tissues or fluids are important. These may include surgical instruments, implanted medical devices, and surgical cloths and fabrics.
These items must be sterile when used because any microbial contamination can lead to infection. Steam is often the disinfectant of choice for sterilizing heat- and moisture-resistant items because it is reliable, compatible, and lethal to microorganisms for employees working on autoclaves.
The difference between industrial autoclave and medical autoclave
Autoclave can be used in a variety of industrial and medical applications. Industrial autoclaves are used in manufacturing environments to process parts and materials using hot steam and pressure: for example, in the manufacture of pressurized wood and special tires used in your car tires.
Autoclaves are also used in scientific research and the pharmaceutical industry – beyond the sterilizing equipment used in laboratory research, most autoclaves are equipped with a liquid cycle to sterilize liquids in the laboratory.
Medical steam disinfectants are used in sanitary environments to sterilize heat and moisture resistant devices such as surgical instruments, implanted medical equipment, and surgical cloths and fabrics.
The cycles used in medical steam disinfection devices are manufactured and approved according to known industry standards.
In the United States, steam disinfectants used in health care must be cleaned by the Food and Drug Administration for the intended use of the disinfectant manufacturer.
Safety items when using an autoclave
An important point to keep in mind when working with an autoclave is that the material should not be removed from the equipment before it dries. Adequate water in the device is very important.
Autoclave is available in different sizes. The smallest and largest is a complex device and we need pre-installation steps to work with it.
Also, do not fill more than three-quarters of the device. Sharp items should not be placed in the autoclave bag. Use waste containers to do this.
Discard as sharp waste. To sterilize the bags in the autoclave, they must be packed freely so that water vapor can flow freely in them.
Glass containers should also be next to them so that air can be easily exchanged in them. Note that the steam does not penetrate the grease, so sterilize the grease in another way. Be sure to use distilled water if the device forms a scale. If you have liquid containers, fill one-third full and leave the rest empty.
Be sure to keep the autoclave in the laboratory. If stored outdoors, be sure to place the device in a non-slip sterile container. This device does not work well at high temperatures, so use the time specified in all instructions. The minimum time required for sterilization is 30-45 minutes. For example, to sterilize working solutions and flasks with minutes and temperatures of 121 degrees. However, more dangerous infectious agents such as culture medium are inoculated and infected samples must be sterilized for one hour.
After sterilizing the samples, first turn off the device and open the steam outlet valve until the pressure inside the device reaches zero. Make sure the door never opens before the autoclave heat and pressure return to normal. When opening the outlet valve, keep your face away from it to prevent burns.
Products related to milk and dairy laboratory >>

Somatic cell counter device
Application: Milk and Dairy Laboratory
Somatic counter counter device for counting milk somatic cells

Caldeal system of digestion and distillation
Application: Milk and Dairy Laboratory
Caldeal system for digestion and distillation to measure protein

Soxhlet device
Application: Milk and Dairy Laboratory
Soxhlet device for measuring fat

Automatic raw fiber machine
Application: Milk and Dairy Laboratory
Raw fiber device for measuring fiber, ADF and NDF

Milk scan machine
Application: Milk Fraud Laboratory
Milk autoanalyzer to detect milk fraud by FTIR method

Valve centrifuge
Application: Milk and Dairy Laboratory
Milk centrifuge to separate fat from milk

Chryscope device
Application: Milk and Dairy Laboratory
Chryscope device for measuring water added to milk
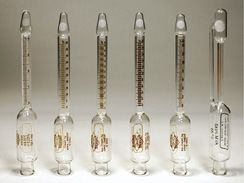
Butterometer milk, cheese and cream
Application: Milk and Dairy Laboratory
Milk butyrometers for milk, cheese, cream and butter

Incubator device
Application: Milk Fraud Laboratory
Incubator for cell and microbial culture

Laboratory chemical hood
Application: Milk and Dairy Laboratory
Chemical hood to remove chemical vapors from the laboratory

Laminar microbial hood
Application: Milk and Dairy Laboratory
Microbial hood for purification and removal of organic agents

Avon-four machine
Application: Milk and Dairy Laboratory
Oven or oven machine for drying laboratory equipment
share



